Bipolar Disorder is a chronic mental health condition marked by intense mood shifts—from extreme highs (mania or hypomania) to deep lows (depression). These changes are far more severe than ordinary mood variations and can disrupt energy levels, behaviour, thinking, sleep, and overall daily functioning. For example, a person may go through a period of unusually high confidence, rapid speech, and reduced need for sleep, and within days or weeks, shift into a phase of exhaustion, sadness, and difficulty concentrating. These unpredictable emotional swings can affect work performance, relationships, and the ability to carry out routine tasks.
Recognising these shifts early and understanding what they mean is important, as proper management can help individuals maintain balance and lead fulfilling, productive lives. This article explores the different types of Bipolar Disorder, key symptoms to be aware of, and effective management strategies that support long-term emotional wellbeing.
What Is Bipolar Disorder?
Bipolar Disorder is a mental health condition characterized by dramatic shifts in mood, energy, and activity levels. These changes are much more intense than ordinary emotional ups and downs. A person may feel unusually energetic, talkative, or confident during a manic episode, often taking on too many tasks or sleeping very little. In contrast, during a depressive episode, they may feel extremely sad, tired, unmotivated, or hopeless, finding it difficult to carry out everyday activities.
These episodes can last for days, weeks, or even months, and the sudden shifts between high and low moods can disrupt work, relationships, and overall quality of life. Despite these challenges, Bipolar Disorder is highly treatable. With the right combination of medication, therapy, routine, and lifestyle support, individuals can manage symptoms effectively and lead stable, fulfilling lives.

Types of Bipolar Disorder
1. Bipolar I Disorder
Bipolar I Disorder is defined by at least one full manic episode that lasts for 7 days or is severe enough to require hospitalization. During this manic phase, the person may show extremely elevated mood, excessive energy, impulsive behavior, or reduced need for sleep. Alongside mania, individuals often experience major depressive episodes that can last for two weeks or longer, bringing intense sadness, fatigue, and loss of interest.
Example:
Rohan goes through a week where he feels unstoppable—sleeping only a few hours, spending money impulsively, talking rapidly, and taking on unrealistic projects. After this high-energy period, he crashes into weeks of deep depression, withdrawing from friends and struggling to function in daily life.
2. Bipolar II Disorder
Bipolar II Disorder is characterized by recurring hypomanic episodes, which are periods of elevated energy and mood that are noticeable but not as extreme or disruptive as full mania. People often feel unusually productive, confident, or talkative during hypomania, but these episodes do not typically require hospitalization. Alongside hypomania, individuals experience major depressive episodes that are often long-lasting, emotionally painful, and significantly impair daily functioning. A key distinction is that Bipolar II does not include any full manic episodes.
Example:
Ananya has days when she feels highly energetic, accomplishes multiple tasks, and talks faster than usual—this is hypomania. But soon after, she falls into weeks of intense sadness, fatigue, and hopelessness, making it hard to work or socialise.
3. Cyclothymic Disorder (Cyclothymia)
Cyclothymic Disorder is a milder but long-lasting form of bipolar disorder. It involves numerous periods of mild hypomanic symptoms and mild depressive symptoms that continue for at least 2 years (1 year in children and adolescents). While the mood changes are not as intense as the full manic or major depressive episodes seen in Bipolar I or II, they are persistent and unpredictable, often causing emotional instability and disruptions in daily life.
Because symptoms are less severe, many people with cyclothymia may not recognise their mood shifts as a mental health condition and may simply describe themselves as “moody,” “sensitive,” or “unstable.” However, the chronic nature of the disorder can interfere with relationships, work consistency, and overall wellbeing.
Example:
Kabir experiences frequent emotional ups and downs for years—days of increased energy and confidence followed by days of low mood or irritability. Although he never reaches full-blown mania or severe depression, the constant mood fluctuations affect his routine and relationships.
4. Other Specified & Unspecified Bipolar Disorders
These categories are used when a person shows clear signs of bipolar-related mood instability but does not meet the full diagnostic criteria for Bipolar I, Bipolar II, or Cyclothymic Disorder. The individual may experience episodes of elevated mood, irritability, increased energy, or depressive symptoms, but the duration, frequency, or intensity may not fit neatly into the established diagnostic patterns.
Despite not fitting the exact criteria, these symptoms can still cause significant emotional distress and disruption in daily life. People in this category often struggle with unpredictable mood swings, functional difficulties, and challenges in maintaining routines or relationships. Proper assessment is important so they can receive appropriate care and support.

Symptoms of Bipolar Disorder
Symptoms appear in two distinct phases:
A. Manic Episode Symptoms
A manic episode is a period of abnormally elevated, overly excited, or intensely irritable mood that significantly affects how a person thinks, behaves, and functions. During mania, energy levels rise sharply, and a person may feel unusually active, confident, or unstoppable.
Common symptoms include:
- Increased energy and restlessness, often moving or talking more than usual
- Reduced need for sleep, sometimes going days with very little rest
- Rapid speech or racing thoughts, making it hard to slow down or stay on one topic
- Impulsive behaviours, such as overspending, risky driving, substance use, or sudden big decisions
- Unrealistic beliefs about abilities or importance, such as feeling invincible or overly powerful
- Irritability or agitation, especially when others try to slow them down
- Difficulty concentrating, jumping quickly between activities or ideas
- Excessive optimism or confidence, sometimes leading to risky or dangerous actions
Real-life Example:
During a manic phase, a person might suddenly start several new projects, spend large amounts of money impulsively, talk rapidly, or stay awake for days feeling “full of energy” and unstoppable.
B. Hypomanic Episode Symptoms
A hypomanic episode is similar to mania but less intense and does not cause major impairment in daily functioning. However, the changes in mood and energy are still noticeable to the person and those around them. Hypomania lasts for at least 4 days and represents a clear shift from typical behavior.
Common symptoms include:
- Increased productivity, often taking on more tasks and working for long hours with unusual efficiency
- Elevated or unusually cheerful mood, sometimes feeling overly confident or upbeat
- Mild impulsive behavior, such as making quick decisions, spending more than usual, or talking faster
- A noticeable change in energy levels, motivation, and activity
- Behaviour that is visible to others, even though it may not cause severe disruptions
Unlike full mania, hypomania does not usually lead to hospitalization or severe consequences, but it can still be a sign of underlying bipolar disorder, especially when followed by depressive episodes.
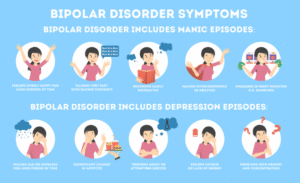
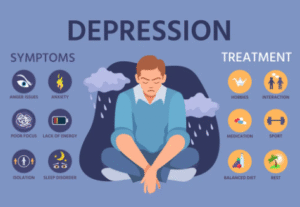
C. Depressive Episode Symptoms
A depressive episode represents the opposite extreme of mania or hypomania. During this phase, energy levels drop significantly, and the person may feel emotionally drained, unmotivated, and disconnected from daily life.
Common symptoms include:
- Persistent sadness or emptiness, often without a specific cause
- Loss of interest in hobbies, work, or activities that once felt enjoyable
- Fatigue or low energy, making simple tasks feel overwhelming
- Changes in sleep patterns, such as insomnia or sleeping excessively
- Changes in appetite, leading to noticeable weight loss or gain
- Difficulty concentrating, slowed thinking, or trouble making decisions
- Feelings of guilt or worthlessness, even when nothing is wrong
- Thoughts of self-harm or suicide, which require immediate attention and support
Real-life Example:
Someone in a depressive episode may stay in bed for most of the day, avoid social interactions, struggle to complete routine tasks, and feel deeply hopeless—even when there is no specific triggering event.
Causes & Risk Factors
Bipolar Disorder does not have a single cause—rather, it develops due to a combination of biological, genetic, and environmental factors. These influences interact in complex ways, increasing a person’s vulnerability to mood episodes.
- Genetics:
Bipolar Disorder often runs in families. If a parent or sibling has the condition, the risk is higher, although not guaranteed. Genetics play a major role in shaping how the brain regulates mood. - Brain Chemistry:
Imbalances in neurotransmitters—such as serotonin, dopamine, and norepinephrine—can affect mood stability, energy, and emotional regulation. These chemical disruptions are strongly linked to manic and depressive episodes. - Stressful Life Events:
Experiences like trauma, the loss of a loved one, financial difficulties, or major lifestyle changes can trigger or worsen symptoms. Stress doesn’t directly cause bipolar disorder, but it can activate underlying vulnerabilities. - Biological Factors:
Hormonal changes, chronic sleep disruption, and irregular circadian rhythms can significantly influence mood swings. Many individuals report that changes in sleep patterns often precede manic or depressive episodes.
Diagnosis
Diagnosis
Diagnosing Bipolar Disorder requires a careful and comprehensive evaluation by a mental health professional, as the condition can often resemble other mental health issues—especially depression. A thorough assessment typically includes:
- Clinical interviews:
A psychologist or psychiatrist discusses your mood patterns, behaviour changes, and emotional experiences over time. - Symptom history:
The professional examines how long symptoms have lasted, how often they occur, and how they impact daily functioning. - Mood tracking:
Keeping a record of mood changes, sleep patterns, energy levels, and triggers helps create a clearer picture of mood cycles. - Family history:
Because bipolar disorder has strong genetic links, understanding whether close family members have mood disorders is an important part of assessment. - Medical evaluation:
Blood tests or physical exams may be conducted to rule out medical conditions that can mimic mood symptoms. - Rule-out of other conditions:
Disorders such as thyroid issues, ADHD, PTSD, borderline personality disorder, or substance use can appear similar to bipolar symptoms. These must be differentiated for accurate diagnosis.
A correct diagnosis is crucial, because Bipolar Disorder is frequently misdiagnosed as depression—especially Bipolar II—leading to ineffective or even harmful treatment approaches. Proper identification ensures the right treatment plan and better long-term outcomes.

Management & Treatment Options
Bipolar Disorder is highly manageable with consistent care.
1. Medication
Medication is often the foundation of treatment for Bipolar Disorder because it helps stabilize mood, reduce the intensity of episodes, and prevent future relapses. Since bipolar symptoms vary from person to person, medication plans are highly individualized.
- Mood stabilizers (e.g., Lithium, Valproate):
These are commonly prescribed to control manic episodes and maintain long-term stability. Lithium, in particular, is considered a gold-standard treatment for bipolar disorder. - Antipsychotics:
Used when symptoms like severe mania, hallucinations, agitation, or rapid mood swings occur. They can also be combined with mood stabilizers for better control. - Antidepressants:
These may be prescribed during depressive episodes but must be used with caution, as they can sometimes trigger mania if not paired with a mood stabilizer.
A psychiatrist carefully designs and adjusts the medication plan based on the person’s symptoms, episode pattern, medical history, and response to treatment. Regular follow-ups are important to monitor effectiveness and manage side effects.
2. Psychotherapy
Psychotherapy plays a vital role in helping individuals understand their condition, recognize early signs of mood shifts, and develop healthier coping strategies. While medication stabilizes the biological aspect of bipolar disorder, therapy addresses the emotional, behavioural, and relational challenges that come with it.
Common therapeutic approaches include:
- Cognitive Behavioral Therapy (CBT):
Helps individuals identify negative thought patterns, challenge unhelpful beliefs, and build practical skills to manage depressive or impulsive behaviours. - Dialectical Behavior Therapy (DBT):
Useful for regulating intense emotions, improving distress tolerance, and developing mindfulness and interpersonal effectiveness. - Psychoeducation:
Teaches individuals and families about bipolar disorder, treatment options, early warning signs, and ways to prevent relapse. Knowledge empowers better self-management. - Interpersonal & Social Rhythm Therapy (ISRT):
Focuses on creating stable daily routines—especially sleep, eating, and activity patterns—to reduce mood swings triggered by rhythm disruptions. - Family Therapy:
Helps family members understand the disorder, communicate more effectively, and create a supportive environment at home.
Psychotherapy enhances emotional resilience, reduces relapse risk, and helps individuals maintain long-term stability.

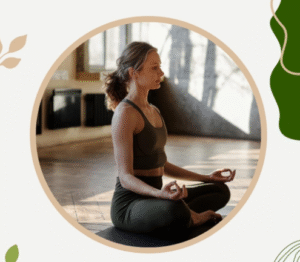
3. Lifestyle & Self-Care Strategies
Lifestyle habits play a crucial role in managing Bipolar Disorder. While they don’t replace medication or therapy, they significantly reduce the frequency and intensity of mood episodes and support long-term stability.
- Maintain regular sleep routines:
Consistent sleep-wake cycles help regulate mood. Irregular sleep is a common trigger for both manic and depressive episodes. - Healthy diet and regular exercise:
Balanced nutrition and physical activity improve energy levels, reduce stress, and support overall emotional wellbeing. Even light activities like walking can help. - Reduce caffeine and alcohol:
These substances can disrupt sleep, increase anxiety, and trigger mood changes, especially in vulnerable individuals. - Track mood changes:
Using a journal or an app to record mood, energy, sleep, and triggers helps identify patterns and early warning signs of episodes. - Limit screen time at night:
Excessive screen use—especially before bed—can interrupt sleep, overstimulate the brain, and destabilize mood rhythms. - Stress management (yoga, breathing, mindfulness):
Relaxation techniques calm the nervous system, reduce emotional reactivity, and help prevent mood swings. - Build a supportive social network:
Staying connected with trusted friends, family, or support groups provides emotional grounding, accountability, and encouragement during difficult periods.
Incorporating these habits consistently can greatly enhance stability and improve quality of life for individuals living with bipolar disorder.
4. Crisis Support
During severe mood episodes, safety becomes the top priority. It’s important to seek immediate help if there are signs of:
- Suicidal thoughts or self-harm urges
- Extreme mania, such as dangerous impulsive behaviour or total loss of control
- Hallucinations or seeing/hearing things that aren’t there
- Aggressive, risky, or unsafe behaviour that puts the person or others in danger
In such situations, professional intervention is essential. Emergency services, crisis helplines, or the nearest hospital emergency department can provide urgent support, stabilize the situation, and ensure safety. Reaching out quickly can prevent harm and provide the immediate care needed during a crisis.

Living With Bipolar Disorder
With proper treatment, many people live stable, productive, and fulfilling lives. Consistency is key—regular medication, ongoing therapy, and balanced lifestyle routines help reduce the frequency and severity of mood episodes while strengthening overall emotional health. Staying committed to a treatment plan is one of the most important steps toward long-term stability.
Support from family, friends, and mental health professionals also plays a vital role in maintaining wellbeing. If you’d like guidance or professional support, you can visit our Counselling Services page to learn more about how therapy can help.
Reference
-
National Institute of Mental Health (NIMH). Bipolar Disorder.
https://www.nimh.nih.gov/health/topics/bipolar-disorder -
American Psychiatric Association. What Is Bipolar Disorder?
https://www.psychiatry.org/patients-families/bipolar-disorders -
Mayo Clinic. Bipolar Disorder: Symptoms & Causes.
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder




















 –Baishakhi Das (MonoProva)
–Baishakhi Das (MonoProva)