Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after witnessing or experiencing a traumatic event—such as violence, abuse, accidents, natural disasters, medical emergencies, or any situation that threatens physical or emotional safety.
While many people feel stressed or shaken after trauma, PTSD develops when the emotional impact stays intense, continues for weeks or months, and begins to affect daily life, relationships, work, or overall wellbeing.
This article explains the core symptoms, how trauma affects the brain, and when to seek help.
Understanding PTSD: Why It Happens
PTSD is not a sign of weakness or inability to cope.
It is the brain’s survival alarm system becoming stuck in danger mode, even when the threat is no longer present.
After trauma, three key parts of the brain are affected:
1. Amygdala — The Fear Alarm
The amygdala becomes overactive, causing:
- Intense fear
- Sudden panic
- Feeling constantly unsafe
Example:
A person who survived a car accident feels a strong fear when hearing a car horn, even if they are safely at home. The brain reacts as if another accident is happening.
2. Hippocampus — The Memory Organizer
The hippocampus helps sort memories and understand timelines. Trauma can disrupt it, leading to:
- Confusing or fragmented memories
- Difficulty recalling parts of the event
- Memories that feel “stuck” or too vivid
Example:
A survivor of a violent incident may remember small details (a smell, a sound) very clearly but cannot recall the full sequence of events. The memory feels scattered and blurry.
3. Prefrontal Cortex — The Rational Thinker
This part helps with:
- Decision-making
- Emotional control
- Understanding safety
Trauma makes the prefrontal cortex less active, so the person struggles to calm themselves even when they logically know they are safe.
Example:
Someone who experienced a medical emergency may panic at small physical symptoms (like a fast heartbeat) even though doctors have reassured them they are healthy.
Why Trauma Responses Affect Thoughts, Emotions, and the Body
Because the brain stays in survival mode, trauma symptoms show up in many ways:
Thoughts
- “Something bad will happen again.”
- “I am not safe anywhere.”
- “It’s my fault.”
Emotions
- Sudden fear or anger
- Emotional numbness
- Deep sadness or guilt
Body
- Tight muscles
- Sweating
- Heart racing
- Stomach pain or nausea
Real-Life Everyday Examples of PTSD Responses
Here are simple, relatable examples to help readers understand trauma responses:
Example 1: Loud Noises
After surviving domestic violence, a person may jump or panic when someone speaks loudly.
Their brain links the volume to danger, even if no threat is present.
Example 2: Avoiding Roads
A person who witnessed a road accident avoids walking near highways or refuses to sit near windows in vehicles.
Example 3: Emotional Numbness
A person who experienced trauma feels disconnected from loved ones.
They smile or behave normally on the outside but feel “empty” inside.
Example 4: Nightmares and Flashbacks
Someone who lived through a fire dreams repeatedly of the flames or smells smoke when there’s no fire.
Example 5: Safety Behaviors
After a burglary, a person checks their doors 3–4 times every night or cannot sleep unless the lights are on.
In Short
PTSD happens because the brain is trying to protect you, but it becomes over-protective.
The mind and body stay on high alert, even when danger is gone.

Core Symptoms of PTSD
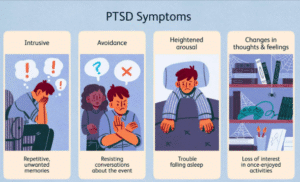
PTSD symptoms generally fall into four main categories. Not everyone experiences all of them, and they can appear weeks, months, or even years after the trauma.
1. Intrusive Memories
Intrusive symptoms are unwanted and distressing experiences that suddenly push the traumatic memory back into the mind, often without any warning. These symptoms make the person feel trapped in the past, even though they are physically in the present.
Common Intrusive Symptoms
1. Flashbacks
Flashbacks feel as if the traumatic event is happening again in real time.
The person may temporarily disconnect from their surroundings and react strongly, thinking the danger is back.
Example:
A person who survived a road accident hears a loud braking sound and suddenly feels as if they are back inside the crash. Their heart races, and they may start crying or shaking.
2. Nightmares Related to the Trauma
Recurring dreams, sometimes exact scenes from the event or symbolic dreams that create fear and panic.
Example:
Someone who experienced a fire may dream repeatedly of burning buildings, smoke, or running to escape—waking up sweaty and terrified.
3. Intense Emotional or Physical Reactions to Reminders
Even simple reminders can cause:
- Rapid heartbeat
- Sweating
- Panic
- Shortness of breath
- Shaking
- Feeling frozen or overwhelmed
Example:
A survivor of emotional abuse may feel panic and breathlessness when they hear someone shouting, even if the argument has nothing to do with them.
4. Intrusive Thoughts or Images
These are sudden, unwanted mental pictures or thoughts related to the trauma.
They can appear during everyday activities like working, eating, or travelling.
Example:
A person who witnessed violence may suddenly imagine the harmful scene again while sitting at their desk or riding a bus.

What Triggers Intrusions?
Intrusions can be triggered by anything that resembles the traumatic event—even if it seems small or unrelated to others. Common triggers include:
- Sounds: sirens, shouting, loud noises
- Smells: smoke, perfume, hospital scents
- Dates or anniversaries: the day the trauma happened
- Visual cues: a similar car, building, or person
- Random moments: sometimes intrusions appear without a clear trigger
Example:
A person assaulted in a dark alley may experience a sudden flashback simply by walking past a dim street or hearing footsteps behind them.
2. Avoidance
In PTSD, the brain’s main goal becomes protecting you from anything that feels dangerous, even if those things are no longer harmful. To achieve this, the mind starts avoiding anything connected to the traumatic experience.
While avoidance may reduce stress in the moment, it prevents healing and often makes symptoms stronger over time.
Common Avoidance Signs
1. Avoiding People, Places, or Situations That Remind You of the Trauma
The person may change routines, skip important events, or stay away from anything that feels similar to the traumatic environment.
Examples:
- After a car crash, someone avoids highways or refuses to sit in a vehicle.
- A person who experienced workplace harassment may avoid the office or feel panic when passing by that area.
- Someone who survived domestic violence avoids crowded or loud places where they feel unsafe.
2. Refusing to Think or Talk About the Event
The mind blocks conversations, thoughts, or memories that feel too painful. This can look like shutting down emotionally or changing the topic instantly.
Examples:
- When someone asks what happened, the person says “I don’t want to talk about it,” or becomes visibly tense.
- They distract themselves with TV, mobile, or work whenever intrusive memories start coming back.
3. Emotional Numbness — Feeling Disconnected From Yourself or Others
To avoid feeling pain, the brain may shut down emotions altogether.
This detachment can look like coldness, lack of interest, or difficulty forming emotional bonds.
Examples:
- A person feels “blank” even during happy moments.
- They find it hard to express love, excitement, or sadness.
- They feel like they are watching life from a distance rather than living it.
4. Using Distractions, Work, or Sleep to Avoid Painful Feelings
People may keep themselves constantly busy or exhausted to avoid facing the trauma.
Examples:
- Working long hours to avoid being alone with thoughts.
- Sleeping excessively to escape emotional pain.
- Overuse of phone, social media, TV, or gaming to avoid thinking about the event.
- Excessive cleaning or overplanning as a way to stay mentally occupied.

Why Avoidance Makes PTSD Worse Over Time
Avoidance provides temporary relief, but it prevents the brain from processing the trauma.
This keeps the fear “unresolved,” and triggers continue to grow stronger.
Eventually, avoidance can:
- Shrink daily life
- Damage relationships
- Increase anxiety
- Strengthen intrusive symptoms
Healing begins when the person slowly learns to face and process the trauma safely—usually with professional support.
3. Negative Changes in Thoughts & Mood
Trauma doesn’t just affect memories—it can also reshape the way a person sees themselves, other people, and the entire world. These changes can feel heavy, confusing, and deeply emotional. Many people with PTSD describe it as “carrying a weight they cannot explain.”
Common Signs of Negative Thought & Mood Changes
1. Persistent Sadness, Guilt, or Shame
These emotions often stay for a long time, even when the person logically knows they didn’t cause the trauma.
Examples:
- Feeling guilty for surviving when others didn’t (“Survivor’s guilt”).
- Blaming themselves for something they couldn’t control.
- Feeling ashamed about how they reacted during the traumatic event.
2. Feeling Emotionally “Flat” or Detached
The person may feel disconnected from their own emotions, relationships, or surroundings.
Examples:
- Not reacting emotionally to good or bad news.
- Feeling like life is happening “far away” or like they’re watching it from outside their body.
- Struggling to form or maintain emotional closeness with family or friends.
3. Loss of Interest in Activities Once Enjoyed
Things that previously brought happiness may no longer feel enjoyable or meaningful.
Examples:
- A person who loved music or art suddenly stops engaging with it.
- Someone who was social becomes withdrawn and avoids gatherings.
- Hobbies, sports, or work no longer feel motivating.
4. Negative Beliefs About Self, Others, or the World
Trauma can rewrite core beliefs, making the world feel unsafe.
Examples:
- “I am unsafe wherever I go.”
- “People cannot be trusted.”
- “I’m weak.”
- “It was my fault.”
- “Something bad will happen again.”
These beliefs may lead to constant fear, self-blame, or low self-worth.
5. Difficulty Experiencing Positive Emotions
Joy, love, or excitement may feel distant or completely absent.
Examples:
- Feeling unable to enjoy family time or celebrations.
- Feeling numb even when something good happens.
- Having trouble expressing affection or happiness.
6. Memory Problems Related to the Trauma
Trauma affects how memories are formed and stored.
People may forget parts of the event or struggle with everyday concentration.
Examples:
- Not remembering important details of the trauma.
- Trouble focusing on conversations or tasks.
- Confusion about timelines (“I don’t remember what happened first”).
Impact on Relationships
These emotional and cognitive changes may cause the person to pull back from others—not because they don’t care, but because they feel too overwhelmed or disconnected.
This can lead to:
- Avoiding friends
- Feeling misunderstood
- Strained relationships
- Reduced communication
Understanding these symptoms helps reduce judgment and encourages compassionate support.
4. Increased Arousal & Reactivity
The nervous system stays on high alert, as if danger is still present.
Symptoms include:
- Irritability, sudden anger, or emotional outbursts
- Hypervigilance—constantly scanning for danger
- Sleep problems (insomnia, restless sleep)
- Difficulty concentrating
- Being easily startled
- Risky or self-destructive behavior in some cases
This “fight-or-flight mode” can be exhausting emotionally and physically.
Common Trauma Responses That Are Often Misunderstood
Many trauma responses are not always recognized as PTSD. These can include:
Emotional responses
- Feeling overwhelmed by small triggers
- Strong guilt or feeling responsible for the trauma
- Emotional numbness or detachment
Physical responses
- Chronic pain or fatigue
- Headaches, stomach issues
- Increased heart rate or breathlessness without medical cause
Behavioral responses
- Social withdrawal
- Misusing alcohol, food, or substances
- Overworking to avoid emotional pain
How PTSD Affects Daily Life
Untreated PTSD can affect:
- Relationships
- Work or academics
- Sleep and physical health
- Decision-making
- Self-esteem
- Overall sense of safety
Many people do not realize they have PTSD because symptoms can appear slowly or be mistaken for anxiety, depression, or anger issues.
When to Seek Help
You should consider professional support if:
- Symptoms last longer than one month
- They disrupt work, relationships, or daily functioning
- You feel emotionally overwhelmed or unsafe
- Nightmares or flashbacks are frequent
- Avoidance is restricting your life
- You feel disconnected, numb, or unable to cope with daily stress
PTSD is highly treatable with the right help.
Therapies like CBT, EMDR, trauma-focused counselling, and mind–body approaches can help you regain safety and emotional balance.
👉 If you need guidance or wish to book a counselling session, reach out here:
Contact Us
Effective Treatments for PTSD
Several evidence-based therapies help individuals process trauma safely:
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
- EMDR (Eye Movement Desensitization and Reprocessing)
- Prolonged Exposure Therapy
- Somatic therapies (body-focused)
- Mindfulness-based therapies
- Medication when needed (under psychiatric guidance)
Early intervention often leads to better recovery.

How to Support Someone With PTSD
- Listen without judgment
- Avoid pushing them to “move on”
- Encourage professional help
- Be patient—healing is not linear
- Help create a safe, calm environment
Final Thoughts
PTSD is a real, valid, and treatable condition. Trauma changes how the brain perceives safety, but with proper therapy, emotional support, and coping strategies, individuals can heal and regain control of their lives.
If you or someone you know struggles with trauma responses, reaching out is the first step toward recovery.
Reference
-
American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
https://www.psychiatry.org/psychiatrists/practice/dsm -
National Institute of Mental Health (NIMH). Post-Traumatic Stress Disorder (PTSD).
https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd -
World Health Organization (WHO). International Classification of Diseases (ICD-11).
https://icd.who.int/en -
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: APA; 2013.
-
National Institute of Mental Health (NIMH). Post-Traumatic Stress Disorder (PTSD).
-
World Health Organization (WHO). International Classification of Diseases, 11th Revision (ICD-11).