In today’s digital age, screens are everywhere—TVs, smartphones, tablets, computers, gaming devices, and even smart toys. While technology offers educational benefits and entertainment, excessive and unregulated screen use can lead to screen addiction, especially in children whose brains are still developing.
Screen addiction is not simply “too much screen time.” It occurs when a child becomes unable to control their use, when screens replace physical activity, social interaction, sleep, and emotional development.
Understanding the risks, recognizing the warning signs, and applying practical solutions can help parents create healthier digital habits and protect their child’s well-being.
What Is Screen Addiction?
Screen addiction refers to the compulsive, excessive, and uncontrolled use of digital devices, where a child feels an overwhelming urge to stay connected to screens despite negative consequences. It can significantly affect the child’s behavior, mood, learning ability, sleep quality, social skills, and overall emotional development.
Unlike adults, children are still learning how to regulate their emotions and impulses, making them particularly vulnerable to digital overuse.
Children are especially at risk because:
✔ Their brain’s reward system is highly sensitive
A child’s developing brain responds strongly to rewards, excitement, and novelty. Fast-moving videos, colorful animations, and gaming achievements trigger dopamine—the “feel-good hormone.”
Over time, the child begins to seek screens repeatedly to experience this quick reward, creating a cycle of craving and dependency.
✔ Digital platforms are intentionally designed to be addictive
Apps, games, and videos use psychological tactics such as:
- Auto-play
- Endless scrolling
- Bright visuals
- Rewards and badges
- Sudden surprises
These design features keep children hooked for long periods, making it difficult for them to stop even when they want to.
✔ Screens become emotional shortcuts for boredom, stress, or loneliness
Instead of learning how to cope with emotions, children may turn to screens as the easiest escape.
They start using devices to:
- Avoid boredom
- Reduce stress
- Distract themselves from loneliness or frustration
This prevents them from developing healthy self-soothing skills, problem-solving abilities, and emotional resilience.
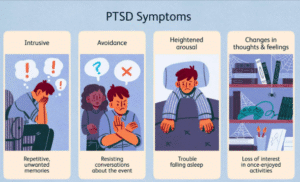
Signs of Screen Addiction in Children
Screen addiction often shows up gradually, and many parents may mistake the early signs as “normal behavior.” However, when screen use starts to interfere with a child’s mood, sleep, social life, and daily functioning, it becomes a cause for concern.
Below are the key indicators, expanded for clarity:
🔸 Behavioral Signs
- Irritability when the screen is removed
The child becomes unusually angry, upset, or frustrated the moment a device is taken away. - Tantrums or aggression over screen limits
Even reasonable boundaries—like turning off the TV or stopping a game—trigger intense emotional reactions or physical aggression. - Sneaking devices or lying about usage
Children may hide tablets, use phones late at night, or lie about how long they’ve been online. - Loss of interest in outdoor play, hobbies, or social interaction
Activities they once enjoyed—drawing, cycling, playing with friends—slowly get replaced by screen time.
These behaviors show that the child is prioritizing screens over real-life experiences.
🔸 Emotional Signs
- Mood swings
The child may shift from excitement to irritability quickly, especially when screen access is restricted. - Anxiety or restlessness without screens
They may constantly ask for the device, seem uneasy during screen-free time, or be unable to relax without it. - Emotional dependence on gaming or videos
Screens become their primary source of comfort, entertainment, or stress relief—similar to an emotional coping mechanism.
This emotional reliance can delay the development of healthy coping skills.
🔸 Physical Signs
- Poor sleep
Blue light overstimulates the brain, leading to difficulty falling asleep or waking up tired. - Eye strain
Dry eyes, burning sensation, or frequent blinking may occur due to prolonged screen exposure. - Headaches
Extended screen use can trigger headaches or migraines in children. - Reduced physical activity
Children become more sedentary, preferring screens over active play. - Poor posture or back/neck pain
Slouching and long hours of sitting contribute to muscle strain and posture issues.
These physical symptoms often appear before parents realize the screen time has become excessive.
🔸 Daily-Life Impact
- Academic decline
Reduced focus and late-night screen use affect school performance and homework quality. - Difficulty concentrating
Fast-paced videos and games can reduce attention span, making sustained focus challenging. - Skipping meals or delaying bathroom breaks
Children may ignore basic needs to continue watching or playing. - Withdrawing from family time
They prefer devices over conversations, meals, or bonding activities.
These daily disruptions show that screen habits are interfering with the child’s overall functioning.
🔸 When to Be Concerned
If multiple symptoms from the categories above are consistently present, the child may be experiencing screen addiction or developing problematic digital habits.
Early intervention—through routines, boundaries, and emotional support—can prevent long-term impact.

Why Children Get Addicted to Screens
Screen addiction does not happen overnight. It develops slowly as children repeatedly turn to screens for entertainment, comfort, or emotional stimulation. Several psychological and environmental factors make children particularly vulnerable:
1. Dopamine Reward System
Games, reels, and cartoons provide instant dopamine hits, which make children feel excited and rewarded. Every time they swipe, win a game, or see something funny, their brain gets a quick burst of pleasure.
Over time, the brain begins to crave this constant stimulation, creating a cycle where the child wants “just one more video” or “one more level.”
2. Emotional Escape
Screens become a shortcut for dealing with emotions. Instead of expressing boredom, frustration, sadness, or loneliness, children escape into cartoons, gaming, or mobile videos.
This prevents them from learning important skills like:
- waiting patiently
- self-soothing
- problem-solving
- coping with negative emotions
3. Lack of Boundaries
When screens are freely available at any time, children naturally use them more.
No rules = no limits.
Without clear boundaries around timing, content, or usage, devices slowly become the dominant activity in a child’s day.
4. Parent’s Screen Habits
Children learn more from what parents do than what they say.
If they see adults constantly scrolling, watching videos, or working on devices, they assume it is normal behavior.
Children may use screens to seek attention or connection if they notice parents are more focused on phones than on interactions.
5. Highly Stimulating Content
Reels, cartoons, and games are designed to be fast-paced, colorful, and highly engaging.
The constant movement, surprises, and bright visuals overstimulate the brain, making slower offline activities—like reading, talking, or outdoor play—feel “boring” in comparison.
6. Social Pressure
Friends, gaming communities, school groups, and online trends all play a role.
Children may feel the need to:
- play games their friends play
- stay updated with trends
- engage in online challenges
- maintain gaming “streaks” or virtual rewards
This peer pressure increases their dependency on screens for social belonging.

Short-Term Effects of Excessive Screen Time
Excessive screen usage can affect children immediately. These short-term impacts often appear within days or weeks and may worsen over time if not addressed.
🔹 Sleep Disturbances
Blue light from screens suppresses melatonin, making it harder for children to fall asleep and stay asleep. Late-night screen use can lead to poor-quality rest and daytime fatigue.
🔹 Reduced Concentration
Fast-paced content overstimulates the brain, making it harder for children to focus on slower, real-world tasks such as reading, homework, or conversations.
🔹 Impulsivity and Restlessness
Constant stimulation from reels, cartoons, and games reduces patience and increases impulsive behavior.
🔹 Eye Strain
Extended exposure causes dryness, burning, blurred vision, and frequent rubbing of eyes.
🔹 Delayed Speech (in toddlers)
Excessive screen exposure replaces caregiver interaction, limiting opportunities for children to learn words, tone, and language patterns.
🔹 Emotional Dysregulation
Children become overwhelmed easily and may struggle to manage frustration, disappointment, or boredom without screens.
Long-Term Effects
If screen addiction continues for months or years, it can significantly affect a child’s physical, emotional, and cognitive development.
🔹 Poor Academic Performance
Reduced focus, lack of sleep, and lower motivation affect school grades.
🔹 Aggression and Irritability
Digital overstimulation and high-intensity gaming can increase mood swings and aggressive responses.
🔹 Social Withdrawal
Children may prefer virtual interactions over real-life friendship, limiting social skill development.
🔹 Delayed Cognitive Development
Too much passive screen time slows down memory formation, problem-solving, and critical thinking.
🔹 Obesity and Low Physical Fitness
Sedentary screen habits reduce physical activity, increasing health risks.
🔹 Reduced Emotional Resilience
Easy access to screens prevents children from building frustration tolerance.
🔹 Problems with Empathy and Real-Life Social Skills
Limited face-to-face interaction hinders emotional understanding and communication skills.

Healthy Screen Time Guidelines (WHO & AAP)
Global health organizations provide age-appropriate recommendations to help parents create balance:
👶 Under 2 Years
🚫 No screen time, except for occasional video calls with family.
🧒 2–5 Years
⏱️ Maximum 1 hour/day, with caregiver supervision and educational content.
👦 6–12 Years
⏱️ 1–2 hours/day, balanced with outdoor play, schoolwork, and hobbies.
👧 Teenagers
⏱️ 2–3 hours/day, with digital boundaries and intentional usage.
Prevention Strategies for Parents
Creating healthy habits early can prevent screen addiction and promote balanced development.
1. Create Daily Screen-Time Limits
Set clear, consistent rules such as:
- No screens during meals
- No screens 1 hour before bedtime
- Pre-decided viewing or gaming slots
2. Model Healthy Digital Behavior
Children learn most from what they see.
- Avoid scrolling during family time
- Put phones away during conversations
- Practice screen-free evenings
3. Build a Balanced Routine
A well-rounded daily schedule keeps children engaged in meaningful activities:
- Outdoor play
- Storytime
- Creative hobbies (drawing, music, crafts)
- Family bonding sessions
4. Use Parental Controls
Enable tools that help manage usage:
- Content filters
- Screen-time trackers
- Safe mode for YouTube & apps
- Password requirement for downloads
5. Encourage Offline Interests
Introduce activities that spark creativity and movement:
- Sports
- Music or dance
- Board games
- Reading
- Puzzles
6. Create Screen-Free Zones
Designate areas where devices are not allowed:
- Bedrooms
- Dining area
- Short car rides
- Study tables
7. Introduce “Boredom Tolerance”
Children should learn that boredom is normal. It develops imagination and problem-solving.
Solutions to Reduce Screen Addiction
If screen overuse is already a problem, these steps can help reverse it:
1. Gradual Reduction Method
Reduce time slowly—about 15 minutes less per week—to avoid major pushback.
2. Replace Screens with Engaging Alternatives
Offer fun, fulfilling options:
- Outdoor sports
- Arts & crafts
- Board games
- Storytelling sessions
3. Create Tech-Free Family Rituals
Build bonding routines that do not involve devices:
- Evening family walks
- Cooking together
- Weekend nature trips
4. Emotional Coaching
Help children identify emotions instead of escaping into screens.
Ask:
✨ “Are you bored, tired, frustrated, or upset?”
This helps build emotional intelligence and resilience.
5. Positive Reinforcement
Encourage healthy habits through appreciation:
- “I love how you spent time outdoors today!”
- “Great job finishing homework before screen time.”
6. Involve Children in Rule-Making
Ask kids to help set limits:
- “How much screen time do you think is healthy?”
When children participate, they follow rules more willingly.
7. Seek Professional Support When Needed
If screen use is affecting:
- Sleep
- Mood
- Relationships
- School performance
A child psychologist can guide behavior change.
When to Seek Professional Help
Consult a mental health professional if your child shows:
- Intense aggression when screens are removed
- Complete withdrawal from offline activities
- Academic decline
- Signs of depression or anxiety
- Behavior problems linked to screen usage
Early intervention helps prevent long-lasting developmental challenges.
Final Thoughts
Screen addiction is rising rapidly, but the good news is that with the right strategies and consistent guidance, healthy balance is absolutely achievable. Children don’t just need limits—they need connection, structure, emotional support, and meaningful offline experiences that enrich their growth. Simply removing screens isn’t enough; what matters is offering fulfilling alternatives that spark curiosity, creativity, and human connection.
By setting clear boundaries, modeling healthy digital habits, and creating a home environment where relationships matter more than devices, parents can help children learn to use technology wisely. These small, consistent efforts support the development of healthy digital habits, stronger emotional regulation, and the ability to build real-life relationships that nurture confidence and resilience.
With awareness and intentional parenting, screen use can become balanced—supporting learning and creativity without compromising emotional well-being.
Reference
1. WHO – Screen Time & Child Health
https://www.who.int/news/item/24-04-2019-to-grow-up-healthy-children-need-to-sit-less-and-play-more
2. American Academy of Pediatrics – Media Guidelines
https://www.aap.org/en/patient-care/media-and-children/
3. Harvard University – Developing Child
https://developingchild.harvard.edu/
Contact for counselling/therapy → contact-us